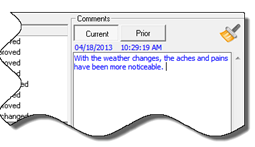
In the upper right corner of the Subjective Complaints screen is an area for Patient Comments (figure 13).
Figure 13
Anything determined to be important can and should be entered in Patient Comments and it will be added to the Subjective area of the final SOAP note. It is critically important to enter anything the patient states on each visit in order to comply with State Board and Federal regulations that require uniqueness in every SOAP note for each and every visit.
The entries made in the Patient Comments Current Tab (figure 13) are saved in the Patient Comments Prior Tab (figure 14). This provides a scroll bar to review all the past comments that have been entered.
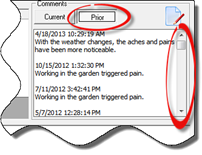
Figure 14
In the upper right corner there is an Edit Icon. Click the Edit Icon to enable Comments entered on prior dates to be edited. The Patient Comments Editor (figure 15) opens with a list of all the Comments on the left. Select the Comment to be edited and it appears in the Comment Detail box on the right.
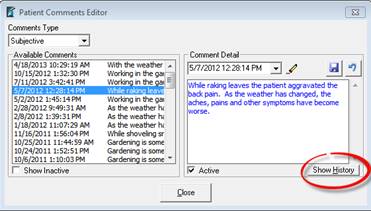
Figure 15
Once the Patient Comments Editor is open, the Comment Detail may be changed in any manner desired. Save the changes by clicking on the Save icon.
Note that each and every change made in the Comment Detail will be fully displayed when the Show History button is clicked. A record of the change will also appear in the EHR Audit Log. The bottom line is that if you make changes, insurance auditors will be able to find and know about them.