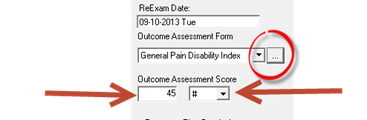
Although this requirement was instituted by Medicare, it has been adopted by many State Boards and other insurance programs. The requirement is that at the time of each examination or re-examination that the patient fills out a Functional Outcome Assessment form. Medicare requires proof, usually in the form of the patient’s signature, that the patient is the one that completed the form. Just below the Re-Exam Date box is the Outcome Assessment Form selector (figure 6).
Figure 6
Click on the drop down arrow to select the form that was completed by the patient on this visit. Under the form selector, enter the score that applies in the left Outcome Assessment Score box. On the right, from the selection box, choose either raw number (#) or percentage (%) to identify the type of grade from the Outcome Assessment form that was used.
The list of forms in the Outcome Assessment Form box is easy to edit. To add or delete a form from the box, click on the Ellipsis icon to the right of the drop down arrow. This will open the Modify List box. To add a form to the list, click the New button at the upper right. A cursor will appear on the last line, next to the asterisk (*). Type in the name of the form. Click the close button and the item will be saved in the drop down list.
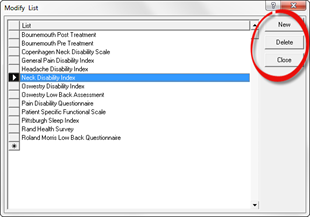
Figure 7
To delete a form from this list click on the Ellipsis icon to the right of the drop down arrow. This will open the Modify List box. Click in the gray space next to the item that is to be deleted so that the item is highlighted. Then click the Delete button. Click the Close button to save the entry.