The Missing Progress Notes report (figure 50) is an audit protector. It empowers the practice to perform a self-audit long before an insurance carrier could do it. It works only when the complete ChiroSuiteEHR system is in the practice. It requires data from both the ChiroPadEMR and ChiroOffice sections of the system. Remember that one of the first things insurance auditors look for is a lack of documentation, and a missing SOAP note is a gigantic problem.
There are times when charges are entered on a patient when a SOAP note has NOT been created for the visit. The Missing Progress Notes report searches for the patients that have had fees charged in ChiroOffice but there is no SOAP note for that date of service in ChiroPadEMR. Since the federal requirement is that SOAP notes must be completed within 72 hours of the visit, this report provides the tool to complete SOAP notes in a timely fashion. The recommendation is that this report should be run at least once daily.
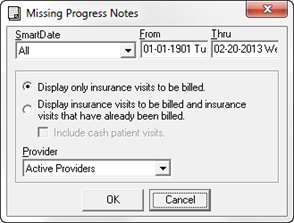
The Selector Pop-Up (figure 49) for the Missing Progress Notes report enables the choice of date or date range, which visits are to be billed, and which Provider the information applies to.
Figure 49
Although many offices opt to Display Only Insurance Visits to be Billed, the recommendation is that the full Missing Progress Notes report should be run. That is, the second selection on the Selector Pop-Up; Display Insurance Visits to be Billed and Insurance Visits that Have Already Been Billed; in addition, place a check in the box to Include Cash Patient Visits. Why? Because auditors have the legal authority to examine ALL patient files to determine whether or not a practice is engaging in illegal billing procedures, such as one fee for insurance claims and a different fee for the same service from cash/self pay patients.
Another item that is looked for by auditors is if the SOAP notes for cash/self pay patients are as fully detailed as the insurance patients. If they are not, the auditors turn the information in to the State Board. In either case, the practice can have many problems if SOAP notes are not completed within 72 hours.
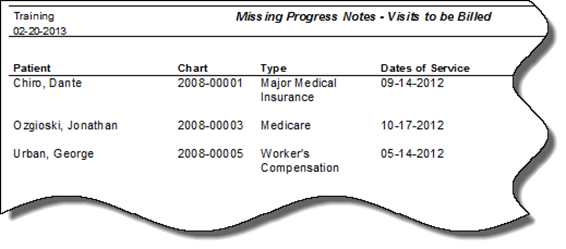
Figure 50
The Missing Progress Notes report should be run daily to verify that all patient notes have been completed.