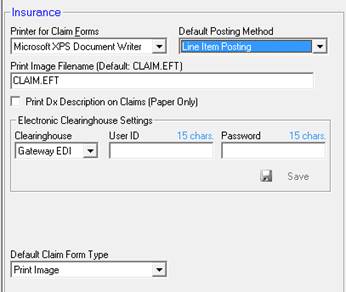
Insurance Preferences are accessed by clicking on the Insurance icon in the dynamic icon bar. Settings affecting insurance claims are changed from this screen, as shown in Figure 9.
Figure 9
Printer for Claim Forms – Whether there is only one printer or multiple printers in the practice, it is required to select the printer that will be used to print the paper CMS-1500 claim forms. Use the drop-down to select which printer installed on your system (defined in the Printers section of the Windows Control Panel) will be used for printing the CMS-1500 claim forms. A laser printer is recommended for insurance claim printing.
Print Image Filename – On this line enter the name of the electronic file that is output when the Print Image or GatewayEDI selection is made for electronic billing. This is the name of the file that will be uploaded to the clearing house for electronic claims. The default that is accepted by most clearing houses is CLAIM.EFT. Note that there are some clearing houses that are not equipped to recognize the .EFT extension. If the practice is working with one of those clearing houses that does NOT accept .EFT, then the extension can be changed to .TXT so that the name of the file becomes CLAIM.TXT or any other name that the clearing house says is acceptable.
Default Posting Method – Choose between Global Posting and Line Item Posting.
•Global Posting is the time saving method which costs the practice precious statistical data. Specifically, for each claim submitted which could be 6 lines of service, there is only 1 payment entry. This means that the practice does NOT know how much the insurance carrier paid for each line item of service, or even if it paid for all line items or just some of them. It involves minimal labor by the office staff, but may cost the practice in uncollected amounts that should have been covered. When is it appropriate to use Global Posting? Possibly in a personal injury (auto accident) case in which treatment of the patient covered a 2 or 3 year period of time during which NO payments had been received. At the time the case settles, there is a single huge lump sum payment which is the final amount. Regardless of the amounts billed, this is all that will be paid, and the insurance carrier may not provide an itemized Explanation of Benefits (EOB). Using Global Posting will greatly speed the entry of this payment on the patient’s Post Insurance window.
•Line Item Posting is the preferred method, although it is much more labor intensive than Global Posting. For each line of service entered on a claim, the insurance carrier typically returns an EOB showing exactly how much was paid for that line item. Line Item Posting means that the staff person enters the exact amount paid on each line item. In this way the practice knows what it is getting paid, whether or not the insurance carrier is paying according to an agreed upon fee schedule, and which services or products are not getting paid. This empowers the practice to place additional claims on the insurance carrier to pay what they are contractually liable to pay. It also makes it possible to determine which services and products should be discontinued.
Print Dx Description on Claims (Paper Only) – Since the most recent revision of the CMS-1500, the verbiage description of a diagnosis is NOT included on the claim form. Currently in ChiroOffice this option applies only to the New York State Workers Compensation forms. When this option is clicked on and selected, ChiroOffice will include the diagnosis description along with the ICD code in box 12 on the New York State C-4.0 and C-4.2 claim forms.
Electronic Clearinghouse Settings is for those offices that have elected to use GatewayEDI as their clearing house for the electronic submission of insurance claims. GatewayEDI has worked with Life Systems Software to integrate some functions to make processing insurance claims easier and simpler. When the practice opts to use GatewayEDI, then from the drop down box select GatewayEDI. GatewayEDI will provide a User ID and Password that must be entered in this section. As soon as the data has been entered in the appropriate fields, click the Save icon in the lower right of this box.
Default Claim Form Type provides a drop down list of the different form types that can be selected for claim submission. Look at the majority of claims submitted by the practice to the insurance carriers. Depending upon how the majority of the claims are submitted to the insurance carriers, the practice should make that method the Default Claim Form Type.
•Most claim forms are submitted on paper, and will continue to be submitted on paper. Select CMS-1500.
•Most claim forms are submitted electronically
o Through GatewayEDI – select GatewayEDI in the drop down
o Through another clearing house – select Print Image
•Most claims are for New York Worker’s Compensation, then select New York C-4