The EHR Audit Log is a Medicare requirement that was designed primarily for the benefits of claims auditors. It is a 2 edged sword. It can protect the practice, or destroy it. The EHR Audit Log tracks all entries made in the system. It identifies the date of the entry, what that entry did (create, delete, edit/modify, etc.), who made the entry and what was the date of the item it applied to. Note that at the time this is being written Medicare, and many State Boards, require that SOAP notes must be completed within 72 hours of the patient’s visit. Any entry in the patient’s file that is made more than 72 hours (3 days) after the visit and is not clearly and properly documented as to what was changed, why it was changed and who made the change will result in charges of fraud. In other words, if the practice does everything the right way, then audits will have no negative effect. If the doctor is in the habit of doing SOAP notes at later points in time, then the time has come to make sure the notes are created in that 72 hour time frame. Ideally, the SOAP notes should be completed before the patient leaves the office.
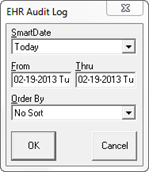
To create the EHR Audit Log, click on the name of the report in the reports menu. This will open the filter pop up for date and sort options (figure 24). Note that the report can be generated for any date or date range that desired, and the sort can be arranged by any of the criteria required in the report.
Figure 24
It is especially important to recognize that the EHR Audit Log identifies the person that made each entry, and this is determined by the Sign-In on that computer. For this reason it is imperative that staff members do NOT share Log-in Passwords.