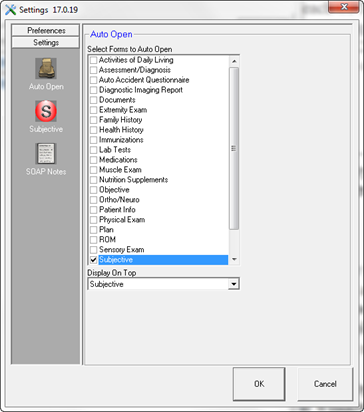
Opening Settings through the ChiroPadEMR section of ChiroSuiteEHR displays Settings that are specific to ChiroPadEMR. In the dynamic button bar, there are 3 icons: Auto Open, Subjective, and SOAP Notes (figure 14).
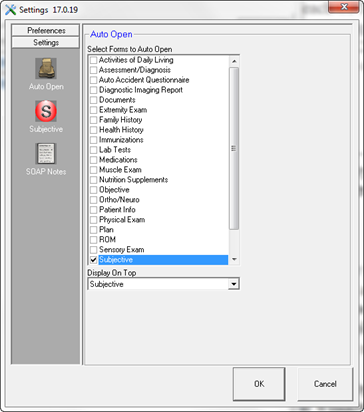
Figure 14
Auto Open empowers the user to select which window in the patient file will be the first one to appear when patient accounts are opened in ChiroPadEMR. Remember that the Settings are computer specific, so each provider or staff member can have ChiroPadEMR open to a different window, depending upon each user’s specific needs. For example, the staff person that updates the patient’s complaints will set it to open to Subjective while the doctor may opt to open to the spinal Objective screen. To make it happen the correct way,
•place a check next to the name of the window that should be the one to open whenever the patient account is opened. Select ONLY ONE window. If more than one window is selected, it will slow down the opening of the patient file.
•In the drop down box entitled Display on Top, select the window name again so it is displayed in the drop down box.
Subjective icon affects the functions on the Subjective Complaint window. See figure 15.
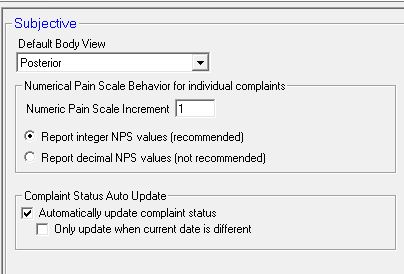
Figure 15
•The first option is for the Default Body View. Choose either Posterior or Anterior and that will be the view that appears every time the Subjective Complaint window is opened. Once it is open you will be able to spin it around to the other view whenever it is needed. The selection of either Posterior or Anterior should be based on the needs of the practice. Specifically, where is the most common location of the complaints that are heard in the practice? If they are usually on the back, then select Posterior; if the complaints are primarily on the front of the body, then choose Anterior.
•Numerical Pain Scale Behavior for individual complaints are settings that apply to the Pain Scale for each complaint.
o Numeric Pain Scale Increment defines the numbers that will appear on the Pain Scale slider bar. If the practice uses the typical 1 to 10 scale, then the number in this box should be 1.
o Report integer NPS values is the recommended selection. This reports the pain scale as a single whole number. It is the easiest to understand and does not raise any questions.
o Report decimal NPS values creates potential issues with insurance examiners because it reports the pain scale with up to six (6) decimal places. For example, the examiners are likely to ask how could the pain scale be so accurate, showing that the patient’s pain level was 6.824691. Although the decimal NPS values were created at the request of some clients, Life Systems Software recommends against using the decimal NPS value scale.
•Complaint Status Auto Update refers to a notification for some complaint Status items that it requires an update. There are 3 possible variations:
o There is NO check in the box labeled Automatically update complaint status. This means that the Update status message does not appear, and that the Status remains as it was entered on the last visit until a user changes it.
o A check is placed in the box labeled Automatically update complaint status. The result is that once the entry is saved and the SOAP note generated, the Status is changed to Update and upon closing the patient file, there will be a message that the Status needs to be updated. Unless the next option is also checked, the Update message will appear even if the patient file is accessed later the same day as the visit.
o When a check is placed in the box labeled Automatically update complaint status another option is made available. The check box to Only update when current date is different will shut off the Update message on the date that the entry was made, but will put it in place on the patient’s next visit date.
SOAP Notes icon enables several options that impact the generated SOAP note in the Documents window. Some of these options should no longer be used due to changes in the laws and regulations of State Boards and the Federal government. See figure 16.
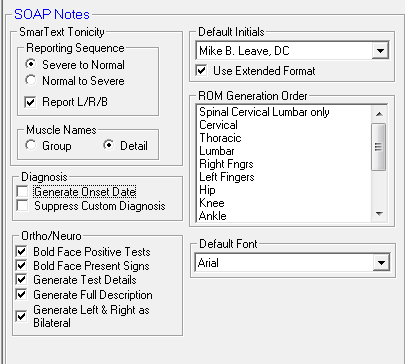
Figure 16
•SmarText Tonicity Reporting Sequence relates to the paraspinal hypertonicity and hypotonicity findings entered on the Objective window.
o Severe to Normal is the preferred selection. It shows a problem from the beginning statement, so claims examiners reading notes are inclined to approve the charges.
o Normal to Severe is technically just as valid as going from Severe to Normal. However, once claims examiners see that something is normal, they have a tendency to assume that everything else is also normal, and then stop reading. The result is a greater likelihood of claims being rejected or denied. Life Systems Software strongly encourages that the user select the Severe to Normal option.
o Report L/R/B determines whether or not the generated SOAP note identifies the tonicity as Left, Right or Bilateral. In order to be compliant with Medicare, State Board and insurance carrier regulations, laws and contracts, it is critically important that this function is turned on by having a check in the box. In the past, depending on technique and personal preference, it was not necessary to report the tonicity findings as left, right or bilateral. The user no longer has this option.
•Muscle Names refers to the paraspinal muscles. When findings of either hypertonicity or hypotonicity are entered on the Objective Spinal Exam window, ChiroPadEMR offers the option of showing either general Group Names (such as Neck Flexors) or specific Detail Names (for example Sternocleidomastoid). Note that some insurance programs may reject claims when reading notes that show only Group Names. Life Systems Software recommends selecting Detail for this setting.
•Diagnosis provides 2 options that affect the generation of the SOAP Note.
o Generate Onset Date looks at the Patient Diagnosis window. See figure 17. If an Onset Date is displayed on the line for a given diagnosis, when this option is checked on, the Onset Date will appear in parenthesis next to the diagnosis in the SOAP Note. To shut off this function, verify that there is no check in the box.
Onset Date in Patient Diagnosis Window
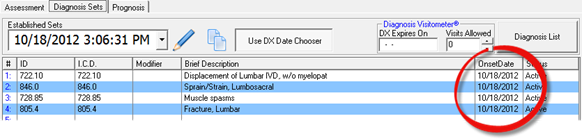
When NOT checked, generates in the SOAP note as:
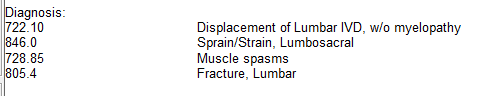
When the Generate Onset Date is checked on, the SOAP note shows:
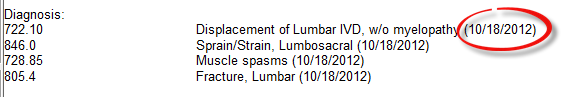
Figure 17
o Suppress Custom Diagnosis is an option requested in the past so that a custom, narrative diagnosis entered in the patient file would NOT appear in the SOAP Note. Under certain circumstances the Custom Diagnosis should be generated ONLY in Narrative Reports and not in the SOAP Note. If the practice falls in this category, then place a check in the box to Suppress Custom Diagnosis. In order for the Custom Diagnosis to be present in the SOAP Note, this option should NOT be checked.
•Ortho/Neuro options determine how the findings for orthopedic tests and neurological signs appear in the SOAP Notes.
o Bold Face Positive Tests is specific for the Orthopedic Tests. Any test that has a positive result will be bold faced in the SOAP Note when this option is checked.
o Bold Face Present Signs is specific for Neurological Signs. Any Sign that is present will be bold faced in the SOAP Note when this option is checked.
o Generate Test Details produces all the test/sign results that have been entered when the check is in the box. If this item is NOT checked, then the findings and results of the test/sign are NOT generated in the SOAP Note. Life Systems Software recommends that this item is always checked and turned on.
o Generate Full Description, when checked the description of the test/sign is added into the SOAP Note. This shows the indications for performing the test and gives a description of how the test/sign is performed. It may also include an explanation of the findings or results of the test.
o Generate Left & Right as Bilateral changes the verbiage in the SOAP Note from “positive on the right and positive on the left” to “positive bilaterally” for each test that has positive findings on both sides. To turn this feature on, place a check in the box.
•Default Initials is a term that dates back to an older era when only the doctor’s initials were required at the end of the SOAP Note. Federal and State laws and regulations now require that the doctor’s full name and credentials appear at the end of each and every SOAP Note. In order for this option to work, each provider in the practice MUST enter his/her full name with credentials in the Initials box in the Provider Catalog. Once the Initials have been saved in the Provider Catalog, then this drop down selection box will be populated. For this computer, choose the Provider’s Initials from the list.
o Use Extended Format - In order to be compliant with Medicare and many State Boards there MUST be additional information that accompanies the Initials. Specifically, at the end of each SOAP Note it must clearly state “Electronically Signed By [doctor’s initials and credentials] [date] [time].” Place a check in the box to Use Extended Format so that this is entered automatically and appears at the end of each SOAP note as show in figure 18.
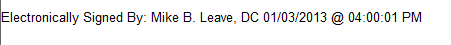
Figure 18
•ROM Generation Order lists ALL the Range of Motion tests in ChiroPadEMR. This box empowers the Provider to arrange the sequence of the tests, that is, the order in which they will appear in SOAP Notes. Using the left mouse button, point at a specific Range of Motion item, hold the button down, and drag the item either up or down the list. When it is in the location desired, release the left mouse button. Repeat the process until all the Range of Motion items are in the order desired.
•Default Font lets the user of this computer select which font will be used to produce the ChiroPadEMR SOAP Notes. Life Systems Software recommends that a common font be selected. The reason for this is an electronic consideration. If the notes are sent to another doctor or health care facility, either by email, HL7 transmission, or on a CD, then that other doctor or facility needs to have the same font on his/her computer in order to see and reproduce the note in a legible format.